PICO Questions
A big part in the process of practicing evidence-based medicine is the gathering of clinical evidence to understand the options and best routes of care health professionals can recommend to achieve the outcome their patients desire. Once that evidence is gathered, and assessed, health professionals combine that research evidence with their own skills and knowledge, and the patients' preferences to formulate the best path forward.
To successfully complete the first part of this process, health professionals should develop a research strategy based on their central clinical question. This initial question will help inform the other areas of this research process so having a clear well-built question from the onset will make the process easier and helps guide searching for evidence-based answers.
There are generally four components of a good clinical question and they are represented by the acronym PICO.
P - Patient, population or problem of interest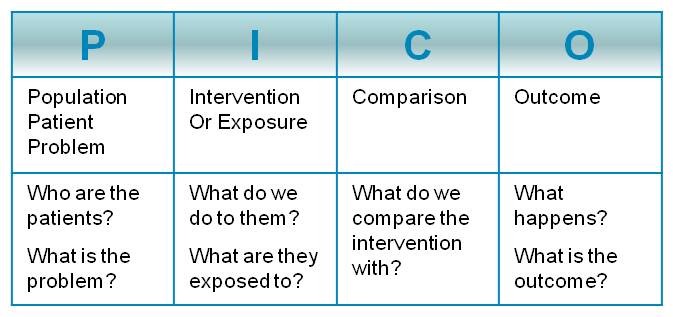
I - Intervention - therapy, prognostic factor, or exposure
C - Comparison intervention, if relevant
O - Outcome(s) of interest
*image from NT Health Library Services http://library.health.nt.gov.au/EBP/questions
Example PICO Questions
Use the four PICO components to formulate a clinical question that can subsequently be used to search relevant search engines and databases in biomedical literature.
Some examples of PICO questions are:
1. In hospitalized patients (P) does the use of non-skid footwear (I) help decrease the number of patient falls (O) compared to patients not wearing non-skid footwear or in bare feet (C)?
2. For adults (18-65) with type 2 diabetes (P), can a regimen of regular aerobic exercise (I) lower levels of glycosylated hemoglobin (O)?
3. Can the use of a treadmill (I) help post-stroke patients (P) improve their mobility and walking coordination (O)?
4. Among term/near term newborn infants born to mothers with risk factors for neonatal infection (P), does the use of immediate prophylactic antibiotic (I), compared to selective use of antibiotics (C) have an impact on neonatal mortality and/or on neonatal sepsis (O)?
5. In low-birth-weight/pre-term neonates in health facilities (P), is skin-to-skin contact immediately after birth (I) more effective than conventional care (C) in preventing hypothermia (O)?
6. For children aged 2–59 months with non-severe pneumonia and wheeze (P), should antibiotics (I) be given to reduce symptoms (O)?
*examples 4-6 adapted from: Recommendations for Management of Common Childhood Conditions: Evidence for Technical Update of Pocket Book Recommendations: Newborn Conditions, Dysentery, Pneumonia, Oxygen Use and Delivery, Common Causes of Fever, Severe Acute Malnutrition and Supportive Care. Geneva: World Health Organization; 2012. ANNEX 2, List of PICO questions. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138330/